Many practitioners are presented with conflicting guideline recommendations and continued debate regarding women’s breast health and screening. At the same time, many patients are inundated with misleading information, which may propagate fear and misunderstanding about mammography. This article aims to provide context and hopefully empower practitioners to have confident and informed conversations with their patients, as well as with the women in their lives.
Beginning in 2009, the United States Preventative Services Task Force (USPSTF) issued a report recommending screening mammography begin at age 50 versus age 40 for average risk women. This was based on costcontainment and initially met with bold criticism by professional organizations. With time, several organizations have modified their recommendations, mostly suggesting a woman and her practitioner make a shared decision regarding screening between the ages of 40-50. This may sound reasonable, but I would offer this is easier said than done. How the conversation is interpreted often leads the patient to take emphasis away from the importance of screening and to find it more convenient to wait. Consider in 2017, 62,130 women ages 49 years and younger were diagnosed with breast cancer in the US. This population made up 19.6% of all breast cancers diagnosed that year, and accounted for 11% of all deaths. Movements such as the “40 not 50” initiative encourage this cohort to pursue screening, and for good reason. Breast cancers diagnosed at an earlier age, are typically more aggressive and have poorer outcomes.
Most recently, debate has focused on the use of 3D mammography, also known as tomosynthesis. As New Hampshire residents, we are fortunate to live in a state with a mandate for insurance companies to cover 3D-tomosynthesis as part of a woman’s routine screening. Many women are not aware of this legislation and are often unaware of the technology being used at time of screening. 3D mammography is able to detect small cancers, particularly in dense breasts which are notoriously challenging to evaluate. It also reduces the rate of false positives or “call backs.” As a breast specialist who treats breast cancer every day, I consider 2D mammography alone to be a disservice to patients, particularly in the setting of dense breasts. The National Comprehensive Cancer Network (NCCN) sets breast cancer management standards and continues to firmly recommend annual screening beginning age 40. The CMC Breast Care Center stands by this recommendation and strongly supports the use of routine, low-dose 3D tomosynthesis.
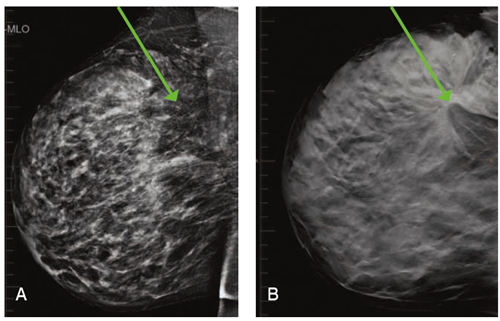
These images illustrate the case of a 49 year old woman who had never undergone 3D screening. They show the striking difference between 2D (A) and 3D (B) imaging. Dense breast tissue appears white on mammography and obscures masses. 3D technology allows us to "scroll through" the layers of the breast to identify distortion and mass-like change. In the 3D image (B) the mass is noted with a green arrow, and the surrounding distortion it is causing is impressive to the trained eye. Diagnostic evaluation showed her tissue to be so dense, even a targeted ultrasound was difficult to delineate the mass. Fortunately, we have 3D stereotactic biopsy capabilities, which allowed us to ultimately diagnose a large and aggressive tumor within the right breast. This came only weeks after she had been told her right breast was normal at an outside institution (based on 2D imaging alone).
References
- American Cancer Society. Breast Cancer Facts & Figures 2017-2018. Atlanta: American Cancer Society, Inc. 2017.
- Breast Cancer Screening and Diagnosis - NCCN Clinical Practice Guidelines in Oncology Version 1.2019 NCCN.org
- Friedewald S. M., Rafferty E. A., Rose S.L. “Breast Cancer Screening Using Tomosynthesis in Combination With Digital Mammography,” JAMA311(2014): 2499-2507.